Locations

Fax: (303) 762-9292

Explaining Spinal Disorders: Lumbar Disc Herniation
A lumbar (low back) disc herniation is a common problem. Descriptive terms for a disc herniation include slipped or ruptured disc. Herniated discs are regularly treated in our practice.
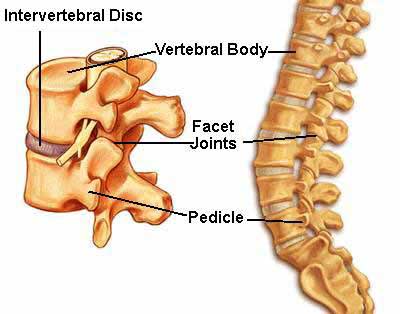
A lumbar herniated disc is a common cause of low back and leg pain (i.e. sciatica). Intervertebral discs, which act as the spine's shock absorbers, are located in between each vertebra. A tire-like band (annulus fibrosis) encases a gel-like substance, the nucleus pulposus.
Symptoms
Symptoms of a lumbar disc herniation may include:
- Dull or sharp low back pain intensified by bending, coughing, sneezing, or other movement
- Muscle spasm or cramping
- Sciatica (pain, burning, tingling, and numbness that extends from the buttock into the leg or foot)
- Leg weakness or loss of leg function
How Does a Disc Herniate?
If the disc's outer band cracks or breaks open, the gel inside the disc can leak out causing a herniated disc. The disc material may place pressure on nearby nerve roots or the spinal cord. Additionally, nuclear material releases chemical irritants causing nerve inflammation and pain.
Sudden stress, such as from an accident, can cause a lumbar disc herniation. Sometimes, a disc herniation develops gradually over weeks or months.
Stages of Disc Herniation
1. Disc Degeneration: chemical changes associated with aging causes discs to weaken, but without a herniation.
2. Prolapse: the form or position of the disc changes with some slight impingement into the spinal canal. Also called a bulge or protrusion.
3. Extrusion: the gel-like nucleus pulposus breaks through the tire-like wall (annulus fibrosus) but remains within the disc.
4. Sequestration or Sequestered Disc: the nucleus pulposus breaks through the annulus fibrosus and lies outside the disc in the spinal canal (HNP).
Factors that can increase the risk for disc herniation include:
- Aging. As you grow older, discs gradually dry out, losing their strength and resiliency.
- Lifestyle choices. Lack of regular exercise, not eating a well-balanced diet, being over-weight, and tobacco use substantially contribute to poor disc health.
- Poor posture, incorrect and/or repetitive lifting or twisting can place additional stress on the lumbar spine.
Diagnosis
Our comprehensive diagnostic process includes:
- Medical history. You doctor talks to you about your symptoms, their severity, and treatments you have already tried.
- Physical examination. You are carefully examined for movement limitations, balance problems, and pain. During your exam, the doctor evaluates loss of extremity reflexes, muscle weakness, loss of sensation, or other signs of a neurological problem.
- Diagnostic tests. Generally, the doctor starts with plain x-ray films, which help rule out other problems such as a tumor or infection. CT scans and MRIs are performed to obtain more detail about your spinal problem.

MRI showing herniated lumbar discs

MRI sagittal (side) view of a large disc herniation of L5-S1
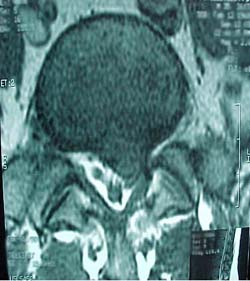
Above: The same disc herniation shown on an axial (overhead) MRI. Note the displacement of the nerve sac by the dark grey / black disc material.
Nonoperative Treatment
Most lumbar disc herniations do not require surgery. Long-standing evidence suggests that pain associated with a herniated disc often diminishes without surgery within 4-6 months.
In fact, 80% of herniated discs get better on their own, without the need for surgery - and improve about 3 months after the onset of leg pain.
Unfortunately, it is not possible to predict which cases will have natural resolution, and which will not. There are many nonsurgical treatments to help relieve symptoms. These include:
- Medications, such as an anti-inflammatory to reduce swelling and pain, muscle relaxants to calm spasm, and occasionally narcotic painkillers to alleviate acute pain.
- Heat/cold therapy, especially during the first 24-48 hours.
- Epidural corticosteroid injection(s) may help relieve significant low back and leg pain.
- Physical therapy, which may include gentle massage, stretching, therapeutic exercise, bracing, or traction to decrease pain and increase function.
In conjunction with these treatments, our staff will educate you about healthy posture and proper body mechanics.
Surgical Treatment
If nonoperative treatment not effective, or there is evidence of neurological deficit (i.e. leg muscle weakness, or numbness), we may recommend surgery. The goals of surgery are to decompress nerve structures and stabilize the spine, if necessary.
At the Colorado Comprehensive Spine Institute (CCSI), this is usually done using a minimally invasive, endoscopic approach, and can be performed on an outpatient basis.
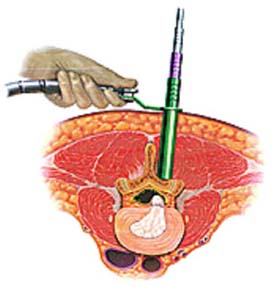 Shown above is placement of an endoscopic cannula (hollow tube) for removal of a herniated disc using a minimally invasive approach. All work is performed through the tube, which is the diameter of a nickel.
Shown above is placement of an endoscopic cannula (hollow tube) for removal of a herniated disc using a minimally invasive approach. All work is performed through the tube, which is the diameter of a nickel.

Above: A lateral (side view) x-ray taken during surgery shows the cannula in place.

Above: Postoperative photo shows two small scars from this poke-hole surgery are barely visible! This patient had a fusion performed through this same approach!
- A discectomy removes either the part of the disc that is compressing nerve structures or the entire disc.
- A laminectomy removes the lamina (vertebral roof) to access disc material from behind that is compressing the spinal canal or nerves. If only part of the lamina is removed, the procedure is a decompressive laminotomy.
- Instrumentation and fusionare performed to stabilize the spine and rarely may be needed in addition to a discectomy. Typically, instrumentation and fusion are needed when there is spinal instability or the disc is severely damaged. Spinal instrumentation and fusion are usually not necessary for a first-time disc, single-level herniation. Fusion may be recommended with a first-time herniation when there is instability, the disc is severely disrupted, or there is a long-standing history of disabling back pain prior to herniation.
Instrumentation (i.e. rods, screws, interbody devices) and fusion (bone graft) joins and stabilized two or more vertebrae. The empty space created by a complete discectomy may be filled with bone graft and a cage, or spacer. There are different types of bone graft, including your own bone harvested from your hip.
Our practice performs many spine surgeries utilizing minimally invasive techniques. At CCSI, unlike many centers, the surgery for disc herniations (decompression or decompression with fusion) is typically done using minimally invasive techniques. Your surgeon will explain your procedure, how it will be performed, along with the benefits and possible risks.
Surgical Recovery
Most patients can begin to get out of bed on the same day surgery is performed to treat lumbar disc herniation. If surgery is performed minimally invasively, the surgery may even be done as an outpatient procedure. Activity is gradually increased and patients are typically able to go home within hours to day(s) after their procedure, depending on the type and extent of the surgery. Expect some pain after the procedure. However, we have pain medications available that will keep you comfortable.
At home, you will need to continue to rest. You will be instructed on how to gradually increase your activity. You may still need to take the pain medications for a while. However, pain and discomfort should begin to reduce within a week or two after surgery. We will discuss with you other techniques for reducing pain and increasing flexibility before you leave for home. We will also discuss with you a timeframe for when you can resume basic activities such as walking, driving and light lifting, and when you can return to more advanced activities such as work, sports and yard work.
At our practice your return to health is our primary concern. If you have any questions about your condition, your treatment, or your recovery, do not hesitate to call us.