Locations

Fax: (303) 762-9292

Explaining Spinal Disorders: Cervical Stenosis
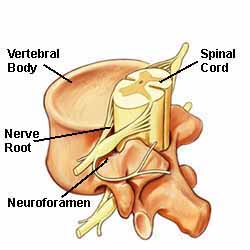
Cervical stenosis develops when either the spinal canal or nerve passageways (foramen) become narrow. It is a common cause of neck pain. If the spinal canal is narrowed, the disorder is also termed cervical central stenosis. If the foramen, or the lateral (side) corners of the spinal canal, is narrowed, it is called cervical foraminal stenosis. When either condition develops, the spinal cord and/or nerves are compressed. Sometimes, patients have both types of cervical stenosis.
Some patients are born with this narrowing (congenital). However, most cases of cervical stenosis develop in patients over age 50 and results from aging and wear and tear on the spine.
Many patients with cervical stenosis have a history of neck injury or trauma. Trauma may have occurred months or years before the onset of stenosis symptoms.
Symptoms
The symptoms of cervical spinal stenosis may include:
- Neck pain; not always severe
- Pain, weakness, or numbness in the shoulders, arms, and legs
- Hand clumsiness
- Gait and balance disturbances
- Burning sensations, tingling, and pins and needles in the involved extremity, including the top of the shoulder, shoulder blade area, upper and lower arm or hand.
- In severe cases, bladder and bowel problems
- Although rare, severe cases can cause loss of function or paraplegia
Diagnosis
Our comprehensive diagnostic process includes:
- Medical history. Your doctor talks to you about your symptoms, their severity, and what treatments you have already tried.
- Physical examination. You are carefully examined for movement limitations, balance problems, and pain. During the exam, the doctor evaluates loss of extremity reflexes, muscle weakness, loss of sensation, or other signs of a neurological problem.
- Diagnostic tests. Generally, doctors start with plain x-rays, which help rule out other problems, such as a tumor or infection. CT scans and MRIs (below) are performed to obtain more detail about your spinal problem, such as evidence of a herniated disc or osteophytes (bony growths). Sometimes, Myelography is performed. Myelography involves injecting contrast dye into the spinal column to visually enhance areas where the spinal cord or nerve roots may be pinched.

Sagittal MRI (above) of a 50-year-old with cervical disc herniations (black protrusions) and cervical stenosis at 3 levels. This view is of the side of the neck with the patient looking left. The general narrowing is the stenosis. Note the compression of the spinal cord (white). This patient has neck and arm pain with numbness, weakness, and leg weakness with walking.
Nonoperative Treatment
Many different nonsurgical treatments help relieve symptoms. These include:
- Medications, such as an anti-inflammatory to reduce swelling and pain, muscle relaxants to calm spasm, and occasionally, narcotic painkillers to alleviate acute pain.
- Cold/heat therapy, especially during the first 24-48 hours of pain onset. " Spinal injections (i.e. epidural) may help relieve neck and related upper extremity pain.
- Physical therapy, which may include gentle massage, stretching, therapeutic exercise, bracing, or traction to decrease pain and increase function.
- Alternative therapy (i.e. acupuncture).
- Typically, manual therapy or chiropractic manipulation is NOT recommended for cervical stenosis.
In conjunction with these treatments, our staff will educate you about healthy posture and proper body mechanics.
Surgical Treatment
If nonsurgical measures are not successful, surgery may be recommended.
There are different surgical techniques to treat cervical stenosis. The goal of surgery is to decompress, or take pressure off the spinal cord and nerve roots. Decompression involves removing or trimming whatever is causing compression. Your surgeon will discuss the best procedure for you, as well as explain the benefits and risks.
- Decompressive laminectomy is a common surgical procedure to treat cervical stenosis. This procedure removes the lamina (vertebral roof) to create more space in the spinal canal for nerves. If only part of the lamina is removed, the procedure is a decompressive laminotomy.
- A posterior laminoplasty expands the size of the spinal canal by lifting the lamina on one side. This procedure retains spinal stability and reduces the need for fusion.
- A discectomy removes part of, or an entire disc, such as a herniated disc that compresses nerve structures.
- A foraminotomy enlarges the size of the foramen to decompress nerve roots.
- Instrumentation and fusion are performed to stabilize the spine and may be combined with another procedure, such as discectomy. Instrumentation (i.e. screws, plates) and fusion (bone graft) joins and stabilizes two or more vertebrae.

Cervical Spine Model with Cervical Plate
The procedures listed above are the most common. A different procedure not listed may be recommended by your surgeon.
Surgical Recovery
Most patients begin to get out of bed the same day surgery is performed. Activity is gradually increased and patients are discharged home within a few days after their procedure, depending on the type and extent of the surgery. As with most surgeries, expect some pain after the procedure. Your doctor will provide pain medication to help keep you comfortable.
At home, you need to continue to rest. You are given instructions how to safely and gradually increase activity. Pain medications may be needed for a while. However, pain and discomfort should begin to reduce within a week or two after surgery. Information about other ways to reduce pain and increase flexibility is provided, along with instructions about your return to work and other activities.
In addition treatment, our medical professionals have a deep commitment to patient education. By helping you understand the cause of your condition, we can help you eliminate risk factors and instill spine healthy habits for a lifetime. While you are under our care, our medical staff will provide you with excellent information to help you recover, minimize risk factors, and stay healthy.









