Locations

Fax: (303) 762-9292

Explaining Spinal Disorders: Cervical Myelopathy
Introduction
Cervical myelopathy refers to a constellation of symptoms and signs due to spinal cord compression in the neck. Because symptoms and signs in a patient with myelopathy can be subtle in early manifestations, the diagnosis may easily be missed or incorrectly attributed to “normal” aging process. However, because the natural history of cervical myelopathy is one of stepwise progression, early recognition and treatment is essential for optimal patient outcome before the onset of irreversible spinal cord damage.
Symptoms
Patients present with a variety of symptoms. There may be a generalized feeling of clumsiness of the arms and hands (such as tendency to drop objects), difficulty to work with small objects such as buttons or coins, changes in handwriting, and generalized numbness. Worse prognostic symptoms include instability in walking, increased tripping or imbalance during walking. Family members may comment that the patient walks as if drunk. Patients with severe spinal cord compression may report electric shock-like sensations down the spine or arms when the neck moves in a certain manner.
In the later stages of the disease, the patients may experience a sense of overall weakness of their arms and legs, as well as changes in their bowel and bladder habits. Despite advanced myelopathy, many patients do not experience any neck pain at all, and this may be one reason that the condition of myelopathy is not diagnosed until very late.
- Early signs: Hand clumsiness and handwriting deterioration
- Late signs: Walking imbalance
Pathology
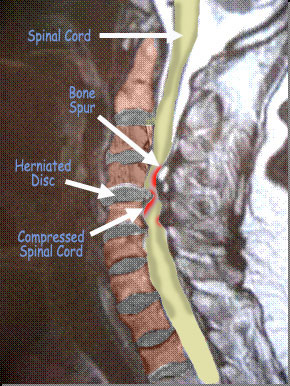
The process of cervical myelopathy is due to compression of the spinal cord in the spinal canal. The physical act of compression, or stenosis, may be a result of different conditions. The most common cause is due to degenerative changes of the cervical spine, known as cervical spondylotic myelopathy. As the cervical spine degenerates, disc herniations or bulges along with arthritic bone spurs can all cause narrowing of the spinal canal, which in turn results in the compression of the spinal cord. Patients who are born with smaller spinal canal diameter (congenital spinal stenosis) have a higher propensity to compress the spinal cord when degeneration occurs. Another condition that results in compression of the cord is known as ossification of the posterior longitudinal ligament (OPLL). In this condition, the ligament in the spinal canal overgrows with abnormal bone, and this in turn causes compression of the spinal cord.
Diagnosis
Abnormal reflexes or subtle changes in a patient’s strength when tested by a medical provider, may prompt them to order further imaging studies to help with diagnosis. X-rays can help delineate whether there is congenital narrowing of the spinal canal, as well as bone spur formations due to degeneration, which may be pressing on the spinal cord. Advanced studies, such as MRI or CT scans with dye, are the tools of choice in confirming spinal cord compression.
Nonoperative Management
Unfortunately, symptomatic myelopathy is a progressive disease resulting in irreversible damage of the spinal cord, and is thus considered a surgical disorder. As we understand more about the pathology of cervical myelopathy, it is now regarded as a surgically condition.
Surgical Treatments
In studies of patients with cervical myelopathy, surgical treatment has been shown to improve functional outcomes, the amount of pain, and neurologic status. It has also been demonstrated that early intervention improves the prognosis by helping to prevent permanent destructive changes of the spinal cord. Surgery is the treatment of choice unless the patient is unwilling or unable to undergo surgery. The goal of surgical treatment for cervical myelopathy revolves around relieving the pressure and compression off of the spinal cord. Depending on the specific mechanism of compression, different methods of surgical treatment may be used to achieve the goal of spinal cord decompression.
Conclusion
Cervical myelopathy is a disorder that is typically treated surgically. Early treatment before the onset of permanent spinal cord injury is recommended. The surgical procedure chosen must be tailored to the patient’s specific pattern of stenosis, comorbidities, and symptoms.
References
Spivak J, Connolly P. Orthopaedic Knowledge Update: Spine 3. American Academy of Orthopaedic Surgeons, Rosemont, IL. 2006.
American Family Physician. 2001 May 15;63 (10):1916.
Figures
MRI of the neck showing multilevel compression of the spinal cord.